In this joint presentation with the World Autism Organization, Frederico Balzola, MD, discusses the intersection of chronic inflammation, gastrointestinal issues, and autism. He considers intestinal permeability and how the microbiome interacts with the central nervous system to affect inflammation in the body. The speaker provides historical context for increased autoimmune and inflammatory diseases and highlights the relationship between GI discomfort/pain and behavioral outcomes. Balzola presents a longitudinal study on inflammatory disease pathogenesis and considers what the results mean for autism medical care moving forward. He summarizes the presentation and critical conclusions before the Q&A.
In this webinar:
4:00 – Disease origin and the gut
8:00 – Intestinal permeability
11:30 – Zonulin and the tight junction
15:40 – Societal changes and the gut
18:10 – Food systems, diet, hygiene, and antibiotics
25:00 – The microbiome and immune responses
30:15 – Fecal Microbiota Transfer therapy
34:00 – Gut inflammation in autism
37:15 – Behaviors and GI discomfort
42:00 – Longitudinal study on GI inflammation in autism
48:40 – Results and interpretation
50:15 – Environmental risks
54:55 – Summary and conclusion
1:02:11 – Q&A
Intestinal permeability
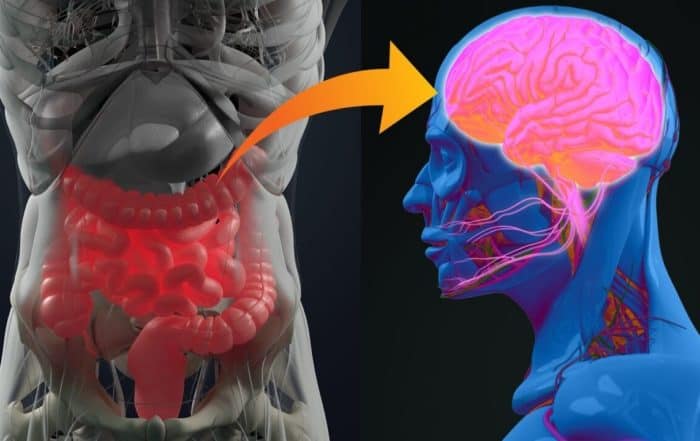
Balzola describes how the prevalence of autoimmune and inflammatory diseases has drastically increased over the last four decades. He asserts that this observation reaffirms Hippocrates’s theory that all diseases begin in the gut (4:00). Dr. Alessio Fasano said (5:50),
“The bowel is a battlefield where enemy and friends negotiate molecular trafficking leading to either tolerance or immune response. It is the largest interface between our body and the outside world.”
The speaker discusses the role of intestinal permeability in immune system function and how increased permeability can lead to chronic inflammation and allergies (8:00). Balzola outlines the structure of the gut lining and details the evolutionary history of the Tight Junction – a group of 150 proteins that regulate the paracellular trafficking pathway from the bowel to the blood vessels (11:30). Zonulin, the first component of the Tight Junction, appeared in humans 2 million years ago, and was a critical step in evolution as it allowed for regulation across the intestinal lining. The Zonulin gene is on chromosome 16 and has been implicated in diabetes, obesity, and several autoimmune diseases (13:50).
Societal changes and the gut
Balzola explains how drastic societal and environmental shifts over the last five decades have driven the increase in autoimmune and inflammatory diseases (15:40). He highlights changes in food systems and processing (18:10), diet and meal size (20:55), hygiene and bacterial exposure (22:35), and antibiotic use (24:05). Each of these changes directly impacts the composition of the microbiome and, therefore, the intestinal lining. Contemporary research shows the capacity of the microbiome to influence immune responses and its implication in liver disease, diabetes, autism, Ankylosing Spondylitis, and other inflammatory and autoimmune diseases (28:00). Researchers have also found specific imbalances in the gut that can upregulate Zonulin release, further suggesting that Zonulin is a trigger for inflammation due to its role in intestinal permeability (29:40).
Gastrointestinal issues in autism
The presenter describes differences in microbiota patterns between autistic and non-autistic individuals (30:15). He touches on fecal microbiota transfer therapy (FMT) and its potential as an effective treatment for gut microbial imbalances in autism and other chronic diseases (31:35). Signs of gut inflammation can be challenging to spot in autistic individuals due to differences in communication and sensory perceptions (34:00). Balzola notes that many autistic people have elevated pain thresholds and difficulties with verbal communication, underscoring the association between behavior and pain expression in autism (36:15). Behaviors commonly associated with gastrointestinal (GI) stress in autism include acid reflux, sleep disturbances, and self-injurious behaviors. The speaker describes possible sitting positions that may help to reduce stomach pain, and illustrates differences in school work outcomes according to levels of pain and inflammation (37:15).
Balzola outlines a longitudinal study with 1650 participants, where 339 autistic individuals had significant GI symptoms. He presents study participants’ initial family history and GI symptom information, noting that 46% had macroscopic malabsorption and 88% had behavioral disturbances after GI symptoms developed (42:00). GI lab examinations for the study included esophagus, stomach, colon, and rectum (44:30). One participant with inflammatory bowel disease and chronic excess of eosinophils (white blood cells) was treated with the FODMAP (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) diet. Results showed a reduction in constipation, abdominal pain, proctalgia, and tenesmus, as well as improvements in hyperactivity, motor skills, and mental attention (48:40). At the one-year follow-up, all symptoms were reduced. Researchers, therefore, conclude that there is a significant association between clinical manifestations and histological alterations, meaning that inflammation induces gastrointestinal diseases and their subsequent behaviors (49:21).
Review and conclusion
The speaker notes that the first 1000 days of life are crucial for clinical inflammatory disease and urges pediatricians to consider this. Environmental risks from pre-conception to postnatal impact inflammatory disease pathogenesis (50:15). He presents a case scenario for cumulative environmental risks, highlighting that the gut microbiome is the result of the sum of every risk and, as such, is very fragile at the beginning (52:30). He summarizes critical points from the presentation and how they translate to changes in perspective and care. Specifically, he urges viewers to consider autism as a multiorgan inflammatory disease and to assume the central nervous system plays a role in intestinal inflammation. He reminds viewers to consider pain thresholds in autistic patients with GI symptoms and to listen to the opinions and experiences of parents to gain a better understanding of autism complexities. Balzola also asserts the need for longitudinal approaches to investigation and medical care to predict and adequately address inflammatory or degenerative diseases (54:55). Most importantly, he continues, it is imperative that evolving information about inflammation in autism is transferred from research to the bedside (1:00:00). He notes Schopenhauer’s three stages of truth before opening to questions (1:01:22).
The speaker:

Take the knowledge quiz
Can’t see the quiz below? Take it online HERE
The Gut, Autism, and Mental Health
Learn about the relationship between the gut-brain axis, mental health, and autism. The speaker: Calliope Holingue, MPH, PhD is a research faculty member at the Center for
New multi-national study adds to evidence linking alterations of the gut microbiome to autism
Strong new evidence linking alterations of the gut microbiome to autism spectrum disorders (ASD) comes from a new multi-national study by James Morton and colleagues. In the study, researchers in North
Constipation in infancy associated with higher likelihood of autism diagnosis
More evidence linking autism spectrum disorders (ASD) to gastrointestinal problems comes from a study by researchers in Taiwan and the United States, who report that ASD occurs at an elevated rate
Microbiota therapy may lead to lasting beneficial changes in the gut health of children with autism
Microbiota transfer therapy (MTT) may lead to long-term improvements in the gut health of children with autism spectrum disorders (ASD), according to a recent study by Khemlal Nirmalkar and colleagues at
Gastrointestinal Symptoms in Autistic Patients
In this joint presentation with the World Autism Organization, Frederico Balzola, MD, discusses the intersection of chronic inflammation, gastrointestinal issues, and autism. He considers intestinal permeability and how the microbiome interacts
Co-Occurring Conditions and Autism
Research suggests that individuals with autism experience some conditions―including underlying medical issues, neurodevelopmental differences, and mental health issues―more frequently than the general population. Learning about these potential medical needs can help you