With 30 years of data supporting growing evidence that dietary intervention is an effective treatment for autism, all too often we hear …
- My doctor says there’s nothing to this diet thing.
- My kid never has diarrhea so he’s not a candidate for the diet
- That diet’s too hard.
- My kid is picky. I don’t want him to go hungry.
- My child could never live without pizza!
- I’m afraid I’ll make too many mistakes – and then it will be my fault.
- The school simply won’t do the diet.
- I don’t want to manipulate their nutrition.
- Children need milk!

Dietary intervention is frequently a component of an evidence-based medical approach, and there is some empirical evidence that special diets help some individuals with autism. This resource includes references, resources, and links for learning more about potentially effective, evidence-based treatments.
Remember: Medical treatments might not be as effective if the diet is not sound, so overcoming these challenges is a crucial first step in meaningful intervention.
Remember also: Your child is an individual. And the only way you are ever going to learn if this is an effective intervention for him/her is to give it an honest trial. Most experts agree that a strict trial of at least three months is needed to determine if a special diet will help. If there are no improvements after three months, you can feel confident that you have made a good try without a major financial investment.
Pitfall #1: Listening to Scoffers
Solution: Historically, many doctors have scoffed at the idea that diet, food additives, sugar, etc. can affect behavior. They believed that there was no supporting scientific evidence. During 2008, this turned a corner, when the American Academy of Pediatrics recognized and published the change.
They now admit,“…we might have been wrong…” This statement, made by the editor of AAP Grand Rounds, refers to the article “ADHD and Food Additives Revisited” by Alison Schonwald. Read online.
Thousands of parents throughout the world have placed their children on special diets and have observed dramatic improvements. You can begin to educate yourself on these dietary options through your own reading and research.
ARI has more than 80 free webinars on nutrition and autism. Access them HERE.
Download ARI’s ‘Science Behind GF/CF Brochure’
Scientific Publications:
- Knivsberg, Wiig, et al. “Dietary Interventions in Autistic Syndromes’ Brain Dysfunction 3 (1990) 315-317
- Knivsberg, Reichelt, et al. “A Randomised, Controlled Study of Dietary Intervention in Autistic Syndromes”
Nutritional Neuroscience 5 no.4 (2002) 251-26
Pitfall #2: Caving in for “Special” Occasions
Solution: Food-oriented holidays and family celebrations can be tricky, but you can say, “My child can’t eat that particular treat, but here’s a great substitute that is okay for him/her.”
- Keep emergency snacks and treats with you.
- Give Grandma/neighbor/school a chance: share a list of “safe treats” ahead of time. That way, others can buy or make them themselves.
- Call hosts, family, friends ahead of time and briefly share your child’s dietary needs. Explain why you need special food, and tell them you will be glad to provide it if that solves the problem.
- Supply food substitutions quietly. If you don’t mention it, others won’t notice and your child won’t feel singled out.
- Educate your child about allergies (therapists, teachers can help) – help them learn to advocate for themselves and make safe choices.
- Remember that special occasion food does not have to be gluten- or casein-based. There are many good, naturally gf/cf foods that are appropriate for every holiday and for all friends and family members.
- Offer to bring “special” foods that are suitable for everyone, for example, bake appropriate cupcakes for all the children at a birthday party, or bring mashed potatoes made without milk to Thanksgiving dinner.
Helpful Resources:
Pitfall #3: Unexpected Exposures in Foods
Solution: Many processed foods contain gluten, wheat germ, (barley) malts, casein, caseinates, whey, and other no-nos in tiny amounts. Read the fine print on the label. However, that isn’t foolproof, so it’s wise to call manufacturers.
If your child reacts or acts up after a meal that included a processed or canned food, be suspicious. Keep a written record, and watch for this to occur again. Not all labels list gluten/casein additives. Examples include canned tuna and salmon, which might contain casein that isn’t on the label. Sometimes ingredients change before the labels do, so if a child reacts to a food that was tolerated previously, call the manufacturer and ask about ingredient changes.
Pitfall #4: Hidden Exposures to Gluten, Casein, and Foreign Substances
Solution: Be vigilant about hidden sources of exposure – for example, hand-to-month ingestion of non-foods can be a real problem. If your child touches homemade playdough (composed primarily of all-purpose flour) and then proceeds directly to snack time without washing hands, gluten can easily be ingested.
Some common exposures parents report include:
- Glue, paste, stickers with adhesive, lickable envelopes
- Toothpaste
- Gum
- Makeup: lipstick, foundation, lotions, etc. (from contact with caregivers’ skin)
- Eating paper
- Play clays and puttys
- Also be aware of inhaled particles, such as: wheat protein in hairspray, flour in the air during baking, etc.
- Pet food
- Crumbs in sofas, food dropped in cars, shopping carts, theaters
- Over-the-counter and prescription medicines
- Cross contamination in kitchens – on the grill, in the fryer, on the slicer, etc.
- Cleaning materials
Note: Although they are not GF/CF diet concerns, it’s crucial to avoid environmental chemical and allergen exposures as well. Use air re-circulation in the car when you can to lower exposure to exhaust, pesticides, etc. In public buildings, particularly schools, work to eliminate use of toxic magic markers, cleaning supplies, chlorine, and flame retardants. Request no idling school busses near the classroom buildings. In the home, avoid pesticide use, use “green” cleaning materials, avoid fragrances, fabric softeners, aerosol products. If the outside air is noticeably polluted, you can filter it using your air conditioner, and keep those filters clean. (And when the outside air is clean, open up your house to ventilation.)
Pitfall #5: Not Understanding Food Sensitivities vs. Food Allergies
Solution: Understand that there are two categories of food allergies: immediate, and delayed reactions.
When most of us think of food allergies we think of an “IgE (immunoglobulin E) response – those that create an almost immediate reaction after eating a problem food. Symptoms include rashes, nasal congestion, coughing, wheezing, closing of the throat, and GI problems from slight nausea to diarrhea. In extreme cases anaphylaxis can occur. Less commonly understood are “IgG” (immunoglobulin G) responses, which can take up to 72 hours to appear. Identifying food sensitivities and removing all potential allergens to minimize challenges to your child’s delicate immune system has been proven to be helpful for many children.
Another problem related to casein and gluten has to do with incomplete digestion, which leads to uptake of possibly harmful peptides (pieces of casein or gluten protein). While not causing a true allergic response, such peptides can lead to behavioral problems.
With autism, we may have other food reactions as well. An example is intolerance to grains, fruits, and vegetables that contain complex sugars of various types. When this occurs it usually is a problem with carbohydrate digestion, leaving undigested sugars in the intestinal tract. Abnormal gut flora can then flourish and cause an inflammatory condition.
Parents suggest: “Get a really thick notebook – in every section put every challenging episode your child has on a scale of 1-10. See red ears? Ear pulling? Cheek rash? Diarrhea or constipation? Write it down. Then every day write down what they ate. Then reconcile the two – figure out if there’s a delayed reaction….”
Pitfall #6: Trusting Products or Restaurants that were GF/CF-friendly in the Past
Solution: Be vigilant; check labels often.
Manufacturers often change ingredients and restaurants can alter recipes.Don’t just wait for announced changes. If you observe a physical or behavioral change in the child, it’s possible they are becoming sensitive to the food – but it’s also possible that an allergen has been added to the food or cross-contamination has occurred. Don’t know what the ingredients are? Call the company.
Pitfall #7: Replacing Casein Products (dairy) with Substitutes
Solution: Be careful when you replace dairy milk with milk substitutes; you need to watch for allergic or other reactions to them.
For example, allergies to soy are very common, as are allergies to nuts. Nuts can also have more oxalates than some people with autism can handle, at least until they get their digestive issues under control. Rice milk can contain complex carbohydrates that cause problems.
See: Jyonouchi H et al. “Evaluation of an association between gastrointestinal symptoms and cytokine production against common dietary proteins in children with autism spectrum disorders” Journal of Pediatrics 2005 May;146(5):605-10.
Pitfall #8: Filling Prescriptions or Buying OTC Medications
Solution: Ask your pharmacist about all ingredients, or, for over-the-counter medications, read the label or call the manufacturer.
Most medications (prescription and OTC) can be compounded – ask your healthcare provider to write prescriptions for compounding, specifying they be allergen-free, and listing those allergens.
Pitfall #9: Replacing Diets with Enzymes
Solution: Deficiencies in digestive factors are extremely common, including essential enzymes (dipeptidylpeptidase 4 [DPP-IV] and others). Determine which enzymes might best help your child; work with an experienced nutritionist, dietitian, or clinician if possible, or use online resources like ARI’s free evidence-based medical approach Diet webcasts to find good options for your child.
Understand their role: Enzymes might be a crucial part of your child’s treatment plan, but they are meant to aid in digestion and most parents report finding they are not a sufficient replacement for a restricted diet. Also, remember that if your child is undergoing medical or nutritional treatment, he/she may be detoxifying – whether the treatment is called detoxification or not. During this time, sequestered toxins can be released and can find their way to the digestive tract where they can impair digestive enzyme activity and cause some degree of (temporary) food intolerance. So it’s a good idea to supplement with a comprehensive blend of digestive enzymes whether your child is on a special diet or not. Realize that digestion and diet can be moving targets while we try to recover our children.
See: “Binding of Infectious Agents, Toxic Chemicals, and Dietary Peptides to Tissue Enzymes and Lymphocyte Receptors and Consequent Immune Response in Autism.” Vojdani, Pangborn et al. Int. J Immunopath Pharm 16 no.3 (2003) 189-199.
Pitfall #10: Thinking it’s a Nutritional Risk to Change a Child’s Diet
Solution: Educate yourself.
- Educate yourself on nutrition, visit the library
- Watch or listen to free ARI webinars
- Get help from a nutritionist or dietitian
- Remember, taking away French fries and hot dogs is taking away – nothing.
- And milk is baby cow food, not really intended for human consumption. Don’t let the milk lobby override common sense.
Pitfall #11: Jumping in too Fast
Solution: Ease your way in. Starting the diet isn’t easy, but you can do it. If your child is young, don’t delay. Typically, younger kids adapt more readily to dietary changes and it’s easier to control their access to food.
You know your child, and you know your own capabilities. Before you do anything else, plan your strategy around both. For many people, cumulative small changes work better than suddenly changing everything. You might start by replacing processed foods with fresh fruits or vegetables, for example. Avoid artificial colors and flavorings. Try replicating your child’s favorite store-bought foods – then gradually change the recipe to healthier ingredients. Sneak the good stuff in. (It’s amazing how easy it is to hide grated carrots!) Make extras and freeze for when you are short on time, or for the babysitter to use. See if you can involve Grandma in this effort; she probably has more time than you do and would like to help. Once she’s helping, she’s enlisted – on your side! Figure out in advance what your specific problems are likely to be – is your child addicted to his favorite foods? Does he dislike certain tastes or textures? Then think through what you are going to do when you hit these snags, and get all the adults in your child’s life to agree to at least try a plan of action. Once you find successful alternatives, the diet becomes much easier.
Also, as with any diet, avoid temptation. Try to not drive by those fast food restaurants that are home to previous bad food choices! At home, keep forbidden foods out of sight and out of reach.
ARI would like to thank Jon Pangborn, Denise Fulton, Kelly Barnhill, Lisa Lewis, Anne Van Rensselaer, Vicky Westlund, Nancy Cale, Denise McMerrick, Janelle Hall, and Matt Kabler for their help assembling the pitfalls.
Learn More About Nutrition & Autism
Building a Healthy Meal Plan
Published: 01/13/2017 Kelly Barnhill, MBA, CN, CCN serves as the Nutrition Coordinator for ARI. She is also Director of the Nutrition Clinic and the Clinical Care Coordinator at the Johnson
Ask the Nutritionist – Live Q&A 2016
Listen to this Q&A with ARI’s Nutrition Director Kelly Barnhill, MBA, CN, CCN. Recorded 12-7-16. Published: 12/07/2016 Ever had a question you wanted to ask a nutritionist? Here's your chance - Kelly Barnhill
Ask the Nutritionist Live Q&A with V. Kobliner, MS, RDN
Because this was a live Q&A, no certificates are offered for this particular recording. Published: 02/25/2015 Vicki Kobliner, MS, RDN has extensive experience using gluten-free, dairy free, low allergen, GFCF, SCD,
Selecting Supplements: Know the Source – V Kobliner, MS, RD
Are you wondering how to pick a good quality supplement? Why do prices vary so much? Is it safe to buy on Amazon? What is
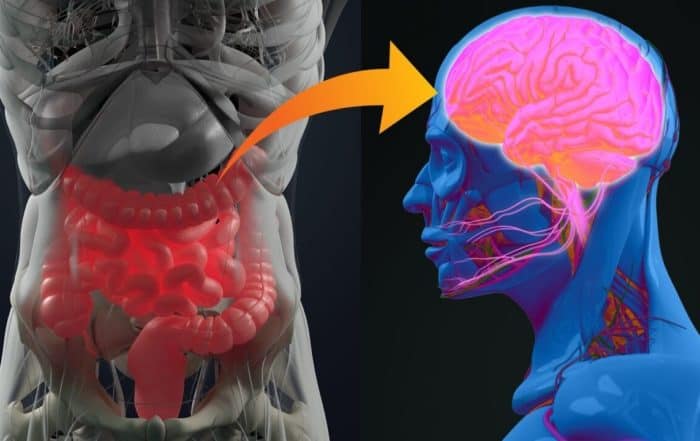
Cross Talk Between Gut & Brain in Autism: Do they understand each other?
Dr. Fasano considers the interplay of environmental factors and the gut microbiome in autism presentation and pathogenesis. He explains intestinal permeability and highlights the role that environmental factors like gluten play in the
Science Behind Nutritional Support for ASD – K Barnhill, MBA, CCN, CN
Recorded November 2013 at Ohio Center for Autism and Low Incidence At first glance, the research behind special diets for autism appears to be mixed, yet parents often insist on trying them.