Some abnormalities seen in autism spectrum disorder (ASD) may be caused by insulin resistance affecting the brain and central nervous system, according to a new study from Italy.
Melania Manco and colleagues note that a number of metabolic anomalies are associated with ASD—for instance, low-grade inflammation, enhanced oxidative damage, low levels of carnitine, high levels of lactate, and high levels of branched-chain amino acids (which are toxic to the central nervous system in excess). The researchers speculate that these abnormalities may be associated with reduced glucose metabolism at the level of the central nervous system, caused by insulin resistance. Insulin resistance occurs when cells do not respond correctly to insulin, a hormone that ferries glucose into the cells, and as a result, cannot obtain sufficient glucose for energy.

The researchers used a test called HOMA-IR to investigate insulin resistance in 60 individuals with ASD between 4 and
18 years of age, comparing them to 240 controls. All of the individuals with ASD were newly diagnosed and had no exposure to psychiatric medications, which can worsen insulin resistance. The researchers note that the HOMA-IR test, in addition to measuring peripheral insulin resistance (for instance, insulin resistance in the muscles), provides an estimate of insulin resistance in the brain.
When the researchers adjusted for sex, age, body mass index, and lipids that are known to influence HOMA-IR, they found that HOMA-IR scores were significantly higher in individuals with ASD.
In addition, they note, 47% of individuals with ASD exhibited elevated levels of branched-chain amino acids, low levels of acetyl carnitine, high levels of lactate, or other metabolic abnormalities. HOMA_IR correlated significantly with levels of BCAAs.
The researchers say the high levels of lactate and low levels of acetyl carnitine seen in individuals with ASD are consistent with dysfunctional activity of the mitochondria (which are the “power plants” of cells). Mitochondrial defects are a common finding in ASD, and the researchers say their findings suggest that brain insulin resistance may impair mitochondrial functioning.
They conclude, “Our study must be intended as [a] provocative attempt at investigating autism as [a] ‘metabolic’ condition in which IR is in some patients the marker of more profound metabolic disturbances that deserve investigation toward a more personalized medicine approach.”
The researchers caution that their study sample was small and that HOMA-IR is a less accurate measure of insulin resistance than “gold standard” measures such as an intravenous glucose tolerance test. Thus, they say, “Findings of this preliminary study suggest it is worth investigating brain glucose metabolism in [a] larger population of patients with ASD by using gold standard technique.”
They conclude, “The recognition of a reduced glucose metabolism in some areas of the brain as a marker of autism might have tremendous impact on our understanding of the pathogenic mechanisms of the disease and in terms of public health.” They also note that a number of interventions that benefit neurotypical individuals with insulin resistance—for instance, dietary interventions, exercise, and drugs such as metformin—might prove to be beneficial for individuals with ASD and insulin resistance.
—
“Cross-sectional investigation of insulin resistance in youths with autism spectrum disorder. Any role for reduced brain glucose metabolism?”, Melania Manco, Silvia Guerrera, Lucilla Ravà, Marta Ciofi degli Atti, Silvia Di Vara, Giovanni Valeri, and Stefano Vicari, Translational Psychiatry, 2021 (free online). Address: Melania Manco, Research Area for Multifactorial Diseases and Complex Phenotypes, Bambino Gesù, Children’s Hospital, IRCCS, Rome, Italy, melania.manco@opbg.net.
This article originally appeared in Autism Research Review International, Vol. 34, No. 3, 2021
ARI’s Latest Accomplishments
Connecting investigators, professionals, parents, and autistic people worldwide is essential for effective advocacy. Throughout 2023, we continued our work offering focus on education while funding and support research on genetics, neurology, co-occurring medical
Biomarkers start telling us a story: Autism pathophysiology revisited
Learn about emerging research on biomarkers and autism from a recent ARI Research Grant recipient. This is a joint presentation with the World Autism Organisation. The presentation by Dr.
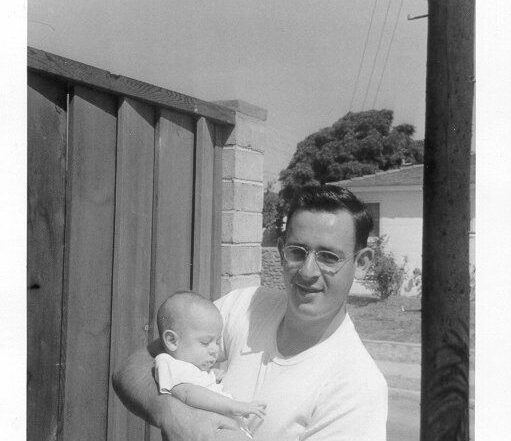
Editorial – Bernard Rimland’s Impact: Sixty Years Since the Publication of ‘Infantile Autism’
In this milestone year of 2024, the Autism Research Institute commemorates the 60th anniversary of Dr. Bernard Rimland’s groundbreaking work, Infantile Autism: The Syndrome and Its Implications for a Neural Theory of