Meltdowns and tantrums present with similar characteristics and are challenging to navigate; however, the root causes of tantrums and meltdowns are very different, and it is crucial to manage them accordingly. Understanding these differences is especially important for individuals with autism spectrum disorder and their caregivers. This article defines meltdowns and tantrums, describes how they differ and provides calming techniques and resources for more information.

Meltdowns vs. Tantrums
A tantrum is an emotional outburst with a specific goal or function. It is a learned behavioral response used to attain the desired outcome (e.g. , get out of an activity, get a toy). Tantrums happen deliberately, and the individual maintains control of their body and mind the entire time. Outbursts generally stop after the desired outcome, so recovery is nearly instant.
Contrastingly, meltdowns are involuntary responses to a nervous system overload. They are the physical manifestation of neurobiological chaos caused by a perceived threat to life. Meltdowns are not behavioral responses and generally aren’t used to attain a specific outcome. The reaction is involuntary and cannot be controlled as intense emotions take over, and tension build-up is released via stimming, repetitive movements, zoning out, screaming, crying, stomping, etc. Once individuals have reached that state, they cannot usually respond to standard behavioral calming cues or techniques. Recovery time for meltdowns can last up to 20 minutes or more after removing the stressor.
Nervous system overload and sensory processing
Difficulties with sensory processing can trigger nervous system overload. Sensory inputs are the first way we interact with and understand the world around us. Our sensory systems (e.g.., touch, smell, sound, sight) automatically process and translate input into meaningful information; however, individuals with impaired nervous systems experience and use sensory inputs differently.
Sensory inputs are perceived and interpreted in the lower part of the brain (brain stem), where our most basic human responses are regulated (i.e., instinct, survival, arousal). The brain perceives highly dysregulated sensory inputs as a literal threat to survival which initiates the fight, flight, freeze response. At that point, sensory information stops transmitting to the emotional processing (limbic system) or analytical (neocortex) parts of the brain, making it very difficult to think about the situation at hand.
Meltdowns and Autism
Many core symptoms of autism are related to sensory processing, communication, and emotional regulation. Differences in brain function and neuron pathway connections may predispose individuals with autism to dysregulated sensory input.
Watch one of our free webinars for more information on sensory processing and emotional regulation in autism:
Sensory Processing and Autism (2019) with Virginia Spielman, MSOT
Emotional Regulation in Autism Spectrum Disorder with Dr. Carla Mazefsky
Sensory Processing and Autism (2015) with Lucy Jane Miller, Ph.D., OTR
Calming and Recovery Techniques
Meltdowns continue until the individual feels safe and calm. They can be challenging to navigate for everyone involved, and it is essential to know what to do when these situations occur. Meltdowns can create uncomfortable or dangerous situations if the stressor continues and proper recovery time isn’t possible. As a parent or caretaker, it is essential to remember that your loved one is experiencing difficulty with their emotions and that they may look to you for support or assistance. Try to take each incident as it comes, and remember to stay calm and provide meaningful support.
Keeping yourself regulated and alert is essential for ensuring your safety and the safety of the individual experiencing dysregulation. You need to meet the individual at their energy level and react quickly to their needs, recognizing when to call for help. A positive response to meltdowns can be simplified into three steps: regulate, relate, and reason.
Regulate
During meltdowns, the emotional part of the brain takes over, and it may be difficult for the individual to listen while they are experiencing it since explanations and logic may not be clearly understood and may add to sensory overload. In these cases, it is best for an individual to self-regulate. Body-based regulations like stimming, jumping, etc., are often purposeful and used as coping mechanisms for sensory imbalances. Use as few words as possible and provide reassurance through self-regulation and calming tools.
It is crucial to stay present with your patient or loved one throughout the entire experience. Some practitioners advise parents to meet their child on their level – if they are jumping and screaming, you can start doing the same thing–sometimes meeting them where they are creates an easier connection. Other times it is best to allow them space for self-regulation. Containment strategies are suggested to defuse meltdowns – mainly when others in the area are in danger. There is no single way to regulate, but maintaining your self-regulation and creating an understanding and supportive presence is important.
Relate
It is equally important to show love and engage your loved one in a supportive situation where they feel safe. Maintain respect and keep in mind that a person in meltdown may be experiencing some trauma from losing control of themselves. It can be an embarrassing and frustrating experience. Let them rest and give them time to calm down and relax. If speaking is possible, tell them it’s okay to feel this way and that it will go away soon. It is essential to be empathetic, validate the experience, and make sure they know they are not alone. If physical contact is okay, tactile, comforting techniques like hugs, weighted blankets, a favorite plush, or a cozy sweater can create a comfortable and safe environment.
Reason
When they have calmed enough to talk (if verbal), try discussing what happened and remind them they are safe. Working through the logic of what happened can help with emotional regulation and personal understanding. Note that this is not a time for lecturing. Remember that a person recovering from a meltdown has just experienced a perceived threat to life and help them to understand what may have triggered that response.
For more tips and resources on sensory supports and meltdown recovery, watch one of these free webinars:
Supporting Sensory Needs with Lindsey Biel, MA, OTR/L
Major Meltdowns: Factors Leading to Emotional Dysregulation in ASD from the Johnson Center
Tantrums and Meltdowns, Oh My! from the Johnson Center
Prevention Strategies and Treatments
Contemporary meltdown treatment and prevention strategies include various therapy and medical techniques. Many approaches incorporate behavioral and physical therapies to help with bodily autonomy and emotional control. Before any treatment or prevention plans are created, your patient/loved one will likely need to complete a Functional Behavior Assessment (FBA) or a similar screening process to identify the functionality of meltdown symptoms.
Creating a behavior log to find patterns in context and surroundings leading up to meltdowns can help the evaluation. Behavior logs also assist parents and caretakers in understanding signs leading up to meltdowns. Learning these timelines allows greater insight into what sensory issues or comorbid conditions may cause meltdowns. Once the context is better understood, you can begin to practice calming techniques before meltdowns occur and teach your loved one or patient to identify their feelings before they happen.
Treating underlying comorbid conditions associated with autism is also essential. Sensory or emotional issues are often the result of uncommunicated pain or discomfort related to such conditions (e.g., GI disruption, anxiety, sleep disorders, etc.). If you have tried cognitive behavioral therapy and meltdown severity or prevalence hasn’t decreased, consider speaking with a gastroenterologist, psychologist, or other medical specialists to address underlying issues.
Watch one of our free webinars to learn more about prevention and treatment techniques:
ABC’s of Behavioral Support in 2021 with Melissa Olive, Ph.D., BCBA-D
Assessing and Treating Challenging Behaviors with Lauren Moskowitz, Ph.D.
Hippotherapy for Autism Spectrum Disorders with Chelsea Whitaker, OTR/L, founder and COO of Taking the Lead
Article: Treating Challenging Behaviors
Article: Supporting Jeremy Home and Community
Meltdowns & Calming Techniques in Autism
Meltdowns and tantrums present with similar characteristics and are challenging to navigate; however, the root causes of tantrums and meltdowns are very different, and it is crucial to manage them accordingly. Understanding
Behavioral Strategies to Treat Anxiety in Individuals with ASD
Lauren Moskowitz, Ph.D. discusses positive behavioral strategies for supporting individuals with autism who also experience anxiety. Handouts are online HERE About the speaker:
Editorial: Challenging behaviors in adults with autism
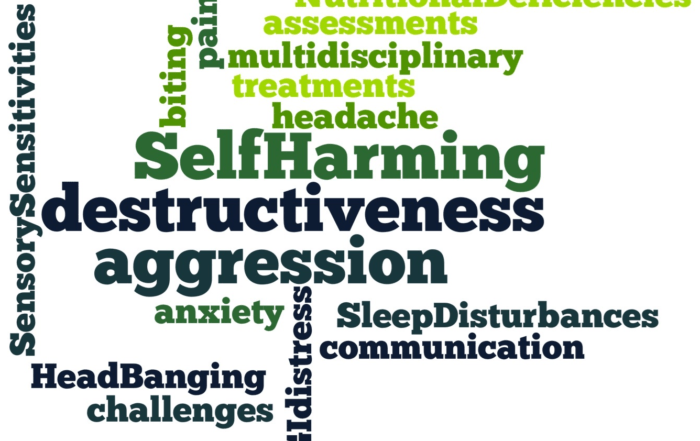
Challenging behaviors such as aggression, destructiveness, and self-injury take a tremendous toll on adults with autism and their caregivers. Each week, the Autism Research Institute receives desperate communications from caregivers seeking help
Self-Injury and Autism – Updates
Listen to playback of this live Q&A as Lauren Moskowitz discusses self-injury and other challenging behaviors. To review Dr. Moskowitz’s previous talk on positive strategies for addressing anxiety and OCD, click HERE
Optimistic Parenting: Hope and Help for Individuals with Challenging Behavior
Handouts are online at: https://ariconference.com/webinars/optimistic.pdf Certificates of Participation are available upon successful completion of a knowledge quiz following the webinar at: https://www.classmarker.com/online-test/start/?quiz=9fd5511d23657ccc Challenging behaviors continue to top the list of concerns for
Toxicant Induced Loss of Tolerance TILT
Handouts are online at: https://www.ariconference.com/webinars/miller.pdf Ebook is online at: https://issuu.com/elisco/docs/tilt_ebook Warning signs of Toxicant-Induced Loss of Tolerance (TILT) – “Does my child have an infection?” or “Is my child allergic?” One hundred fifty